- Alebić, M., Stojanović, N., Baldani, D., & Duvnjak, L. (2017). Metabolic implications of menstrual cycle length in non-hyperandrogenic women with polycystic ovarian morphology. International Journal Of Basic And Clinical Endocrinology, 55(3), 798-807. http://dx.doi.org/10.1007/s12020-016-1062-y
- Ashrafi, M., Fakheri, T., Kiani, K., Sadeghi, M., & Akhoond, M. R. (2014). Impact of The Endometrioma on Ovarian Response and Pregnancy Rate in In Vitro Fertilization Cycles. International Journal of Fertility & Sterility, 8(1), 29–34.
- Ashrafi, M., Sadatmahalleh, S., Akhoond, M., & Talebi, M. (2016). Evaluation of Risk Factors Associated with Endometriosis in Infertile Women. International Journal Of Fertility And Sterility, 11(21).
- Baldani, D. P., Skrgatic, L., & Ougouag, R. (2015). Polycystic Ovary Syndrome: Important Underrecognised Cardiometabolic Risk Factor in Reproductive-Age Women. International Journal of Endocrinology, 2015, 786362. http://doi.org/10.1155/2015/786362
- Balen, A., Morley, L., Misso, M., Franks, S., Legro, R., & Wijeyaratne, C. et al. (2016). The management of anovulatory infertility in women with polycystic ovary syndrome: an analysis of the evidence to support the development of global WHO guidance. Human Reproduction Update, 22(6), 687-708. http://dx.doi.org/https://doi.org/10.1093/humupd/dmw025
- Barthelmess, E. K., & Naz, R. K. (2014). Polycystic ovary syndrome: current status and future perspective. Frontiers in Bioscience (Elite Edition), 6, 104–119.
- Bates, G. W., & Legro, R. S. (2013). Longterm management of Polycystic Ovarian Syndrome (PCOS). Molecular and Cellular Endocrinology, 373(0), 91–97. http://doi.org/10.1016/j.mce.2012.10.029
- Benschop, L., Farquhar, ,., van der Poel, N., & Heineman, M. (2010). Interventions for women with endometrioma prior to assisted reproductive technology. Cochrane Database Of Systematic Reviews, (11). http://dx.doi.org/10.1002/14651858.CD008571.pub2
- Brauner, R., Bashamboo, A., Rouget, S., Goulet, M., Philibert, P., Sarda-Thibault, H., … McElreavey, K. (2010). Clinical, Biological and Genetic Analysis of Prepubertal Isolated Ovarian Cyst in 11 Girls. PLoS ONE, 5(6), e11282. http://doi.org/10.1371/journal.pone.0011282
- Bremer, A. A. (2010). Polycystic Ovary Syndrome in the Pediatric Population. Metabolic Syndrome and Related Disorders, 8(5), 375–394. http://doi.org/10.1089/met.2010.0039
- Byron Redwine, D. (2015). Ovarian endometriosis: a marker for more extensive pelvic and intestinal disease. Fertility And Sterility, 72(2), 310-315. http://dx.doi.org/http://dx.doi.org/10.1016/S0015-0282(99)00211-3
- Choi, P.-W., Yang, J., Ng, S.-K., Feltmate, C., Muto, M. G., Hasselblatt, K., … Ng, S.-W. (2016). Loss of E-cadherin disrupts ovarian epithelial inclusion cyst formation and collective cell movement in ovarian cancer cells. Oncotarget, 7(4), 4110–4121. http://doi.org/10.18632/oncotarget.6588
- Dumitrescu, R., Mehedintu, C., Briceag, I., Purcarea, V., & Hudita, D. (2015). The Polycystic Ovary Syndrome: An update on metabolic and hormonal mechanisms . Journal of Medicine and Life, 8(2), 142–145.
- Dunaif, A. (2016). Perspectives in Polycystic Ovary Syndrome: From Hair to Eternity. The Journal of Clinical Endocrinology and Metabolism, 101(3), 759–768. http://doi.org/10.1210/jc.2015-3780
- El Hayek, S., Bitar, L., Hamdar, L. H., Mirza, F. G., & Daoud, G. (2016). Poly Cystic Ovarian Syndrome: An Updated Overview. Frontiers in Physiology, 7, 124. http://doi.org/10.3389/fphys.2016.00124
- Emeksiz, H. C., Derinöz, O., Akkoyun, E. B., Güçlü Pınarlı, F., & Bideci, A. (2017). Age-Specific Frequencies and Characteristics of Ovarian Cysts in Children and Adolescents. Journal of Clinical Research in Pediatric Endocrinology, 9(1), 58–62. http://doi.org/10.4274/jcrpe.3781
- Ingrid Dravecká, I. (2016). CLINICAL EFFECTS OF SYNDRODE OF POLYCYSTIC OVERS, 65(2), 392-397.
- Iwase, A., Nakamura, T., Nakahara, T., Goto, M., & Kikkawa, F. (2014). Assessment of ovarian reserve using anti-Müllerian hormone levels in benign gynecologic conditions and surgical interventions: a systematic narrative review. Reproductive Biology and Endocrinology : RB&E, 12, 125. http://doi.org/10.1186/1477-7827-12-125
- Kalra, G., Campbell, S., & Nargund, G. (2016). Ovarian reserve may be compromised after adnexal surgery: Are we sufficiently fertility- focused in our surgical training? Facts, Views & Vision in ObGyn, 8(2), 104–108.
- Kim, J. H., Lee, S. M., Lee, J.-H., Jo, Y. R., Moon, M. H., Shin, J., … Jeon, H. W. (2014). Successful Conservative Management of Ruptured Ovarian Cysts with Hemoperitoneum in Healthy Women. PLoS ONE, 9(3), e91171. http://doi.org/10.1371/journal.pone.0091171
- King, J. (2017). Polycystic Ovary Syndrome. Journal Of Midwifery Womens Health, 51(6), 415-422. http://dx.doi.org/https://doi.org/10.1016/j.jmwh.2006.01.008
- KOSOVA, G., & URBANEK, M. (2013). GENETICS OF THE POLYCYSTIC OVARY SYNDROME. Molecular and Cellular Endocrinology, 373(0), 29–38. http://doi.org/10.1016/j.mce.2012.10.009
- Legendre, G., Catala, L., Lacoeuille, C., Boussion,, F., Sentilhes,, L., & Descamps,, P. (2014). Relationship between ovarian cysts and infertility: what surgery and when. Fertility And Sterility, 101(3), 608-614. http://dx.doi.org/http://dx.doi.org/10.1016/j.fertnstert.2014.01.021 show
- Leibson,, C., Good,, A., Hass, S., Ransom, J., Yawn, B., O’Fallon, M., & Melton, J. (2004). Incidence and characterization of diagnosed endometriosis in a geographically defined population. FERTILITY AND STERILITY, 88(2), 314-321.
- Lenart-Lipińska, M., Matyjaszek-Matuszek, B., Woźniakowska, E., Solski, J., Tarach, J. S., & Paszkowski, T. (2014). Polycystic ovary syndrome: clinical implication in perimenopause. Przegla̜d Menopauzalny = Menopause Review, 13(6), 348–351. http://doi.org/10.5114/pm.2014.47988
- Mavrelos, D., & Saridogan, E. (2015). Treatment of Endometriosis in Women Desiring Fertility. Journal of Obstetrics and Gynaecology of India, 65(1), 11–16. http://doi.org/10.1007/s13224-014-0652-y
- McCartney, C. R., & Marshall, J. C. (2016). Polycystic Ovary Syndrome. The New England Journal of Medicine, 375(1), 54–64. http://doi.org/10.1056/NEJMcp1514916
- Nieweglowska, D., Hajdyla-Banas, I., Pitynski, K., Banas, T., Grabowska, O., Juszczyk, G., … Jach, R. (2015). Age-related trends in anti-Mullerian hormone serum level in women with unilateral and bilateral ovarian endometriomas prior to surgery. Reproductive Biology and Endocrinology : RB&E, 13, 128. http://doi.org/10.1186/s12958-015-0125-x
- Palomba, S., Santagni, S., Falbo, A., & La Sala, G. B. (2015). Complications and challenges associated with polycystic ovary syndrome: current perspectives. International Journal of Women’s Health, 7, 745–763. http://doi.org/10.2147/IJWH.S70314
- Pavone, M. E., Hirshfeld-Cytron, J., Tingen, C., Thomas, C., Thomas, J., Lowe, M. P., … Woodruff, T. K. (2014). Human Ovarian Tissue Cortex Surrounding Benign and Malignant Lesions. Reproductive Sciences, 21(5), 582–589. http://doi.org/10.1177/1933719113506498
- Piltonen, T. T., Chen, J. C., Khatun, M., Kangasniemi, M., Liakka, A., Spitzer, T., … Giudice, L. C. (2015). Endometrial stromal fibroblasts from women with polycystic ovary syndrome have impaired progesterone-mediated decidualization, aberrant cytokine profiles and promote enhanced immune cell migration in vitro. Human Reproduction (Oxford, England), 30(5), 1203–1215. http://doi.org/10.1093/humrep/dev055
- Randeva, H. S., Tan, B. K., Weickert, M. O., Lois, K., Nestler, J. E., Sattar, N., & Lehnert, H. (2012). Cardiometabolic Aspects of the Polycystic Ovary Syndrome. Endocrine Reviews, 33(5), 812–841. http://doi.org/10.1210/er.2012-1003
- Sam, S., Scoccia, B., Yalamanchi, S., & Mazzone, T. (2015). Metabolic dysfunction in obese Hispanic women with polycystic ovary syndrome. Human Reproduction (Oxford, England), 30(6), 1358–1364. http://doi.org/10.1093/humrep/dev073
- Santoro, N., Eisenberg, E., Trussell, J. C., Craig, L. B., Gracia, C., Huang, H., … Zhang, H. (2016). Fertility-related quality of life from two RCT cohorts with infertility: unexplained infertility and polycystic ovary syndrome. Human Reproduction (Oxford, England), 31(10), 2268–2279. http://doi.org/10.1093/humrep/dew175
- Şimşek, M., Kuloğlu, T., Pala, Ş., Boztosun, A., Can, B., & Atilgan, R. (2015). The effect of ethanol sclerotherapy of 5 minutes duration on cyst diameter and rat ovarian tissue in simple ovarian cysts. Drug Design, Development and Therapy, 9, 1341–1347. http://doi.org/10.2147/DDDT.S76835
- Tafazoli, M., Fazeli, E., Dadgar, S., & Nematy, M. (2016). The Association of the Dietary Fat and Functional Ovarian Cysts in Women of Reproductive Age Referring to Three Hospitals in Mashhad, Iran, 2014. International Journal of Community Based Nursing and Midwifery, 4(2), 148–156.
- Teede, H., Deeks, A., & Moran, L. (2010). Polycystic ovary syndrome: a complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan. BMC Medicine, 8, 41. http://doi.org/10.1186/1741-7015-8-41
- Tehrani, F., Mansournia, M., & Solaymani-Dodaran, M. (2017). Age-specific serum anti-Müllerian hormone levels: estimates from a large population-based sample. The Journal Of International Menopause Society, 17(5), 591-597.
- van Helden, J., & Weiskirchen, R. (2017). Performance of the two new fully automated anti-Müllerian hormone immunoassays compared with the clinical standard assay. Human Reproduction, 30(8), 1918-2006. http://dx.doi.org/10.1093/humrep/dev127
- Welt, C. K., & Carmina, E. (2013). Lifecycle of Polycystic Ovary Syndrome (PCOS): From In Utero to Menopause. The Journal of Clinical Endocrinology and Metabolism, 98(12), 4629–4638. http://doi.org/10.1210/jc.2013-2375
- Winkelman, W. D., Katz, P. P., Smith, J. F., & Rowen, T. S. (2016). The Sexual Impact of Infertility. Among Women Seeking Fertility Care. Sexual Medicine, 4(3), e190–e197. http://doi.org/10.1016/j.esxm.2016.04.001
- Yuqing, Y., Pei, H., Chang, Y., Chen, M., Wang, H., Xie, H., & Yao, S. (2014). The impact of endometrioma and laparoscopic cystectomy on ovarian reserve and the exploration of related factors assessed by serum anti-Mullerian hormone: a prospective cohort study. Journal Of Ovarian Research, 7(108). http://dx.doi.org/https://doi.org/10.1186/s13048-014-0108-0
- Nasiri Amiri, F., Ramezani Tehrani, F., Simbar, M., Mohammadpour Thamtan, R. A., & Shiva, N. (2014). Female Gender Scheme is Disturbed by Polycystic Ovary Syndrome: A Qualitative Study From Iran. Iranian Red Crescent Medical Journal, 16(2), e12423. http://doi.org/10.5812/ircmj.12423
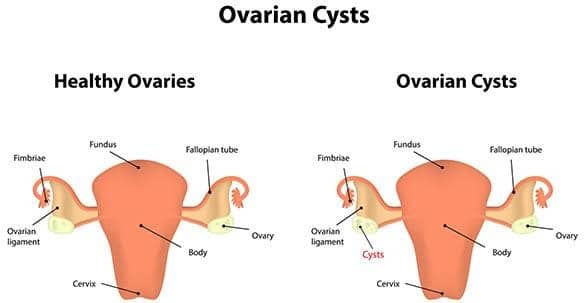
Ovarian Cysts and their Implications on Fertility
Sources
More samples
Related Essays
Get a brand-new guide on essay writing
The download will start within seconds. Good luck!
Download Sample
This essay is publicly available.
Offered for reference purposes only.
Offered for reference purposes only.
By clicking Get this Sample you agree to the Terms And conditions and Privacy policy.
Thank you!
The download will start shortly.